About Seed Implantation
The SPI medical team established the first ultrasound-guided prostate implant program in the U.S. in 1985. We have trained many physicians and assisted in developing programs at many institutions. This is a general guide to prostate brachytherapy, as described at our center. However, many variations in approach and technique have been proven in skilled hands to be highly successful in treating men with prostate cancer.
About prostate seed implants
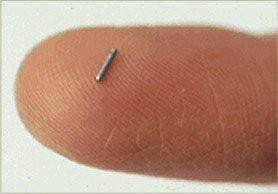
Prostate seed implants are a type of brachytherapy, which translated from latin literally means ‘short therapy’. This describes that the radiation ‘seeds’ deposit their radiation dose over a very short distance. In this technique the seeds are placed directly within the prostate gland. This allows a very high dose to be delivered to the prostate with a fast drop-off of dose outside the prostate, minimizing damage to surrounding structures. Radioactive seeds are about the size of a grain of rice. After delivering their radiation over weeks to months, the seeds are inert and remain in the body.
Initial evaluation
Since the success of an implant depends on the accurate placement of seeds, the first step in treatment process (and evaluation for suitability of an implant) is the volume study. The ultrasound volume study determines the size and shape of the prostate. This is performed in our office and is a relatively simple procedure. An ultrasound probe in inserted into the rectum and moved along the length of the prostate taking cross sectional images every few millimeters. The software calculates the 3D volume after the staff or physician identifies and contours the prostate on the images. Generally, a size of 60 cc’s is the maximum size for a satisfactory implant to be performed. At times, hormone therapy can be initiated two to three months before an implant and the gland will shrink on average by about 30%.
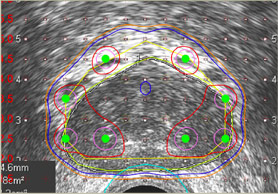
The physician then determines the target volume to be covered by radiation. In general this would include the prostate plus 2-5 mm of tissue surrounding the entire gland. This allows for a margin to treat potentially microscopic cancer cells outside the prostate capsule. Depending on the clinical risk factors, the physician may include more or less extra-capsular tissue in various areas of the gland. Once the volume is determined, elaborate software, a trained radiation dosimetrist, and the physician determine the number, strength, and geometric arrangement of seeds to properly cover the gland. On average, approximately 100-110 seeds are used in a typical implant.
What to expect during the procedure
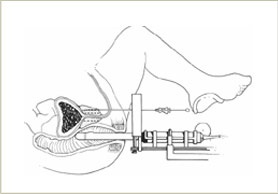
The implant itself is an outpatient procedure. Using a rigid template-guiding device, hollow metal needles containing the seeds are inserted into the prostate from outside the body. At SPI, patients are in the hospital for a total of approximately 5 hours.
In the OR, the physician uses live ultrasound guidance to reproduce the images obtained at the volume study and then inserts needles to the correct depth as seen on ultrasound. Then, the hollow needles are retracted while a metal stylet ‘holds’ the seeds in place. Then both needle and stylet are removed and only the seeds remain. Typical time to perform an implant is just one hour and either spinal or general anesthesia can be used.
After the procedure
 |
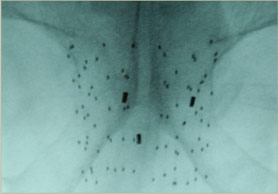 |
After the implant, the patient will recover in the recovery room, and if a Foley catheter was inserted, it will be typically removed. On the day after the implant, a pelvic X-ray, a chest X-ray, and a CT scan are taken. The pelvic x-ray provides the physician confirmation about the implant and aids in counting the seeds. The chest x-ray is often performed to determine if any seeds were deposited into the blood stream and carried to the lungs (this rare event does not appear to cause any harm to patients).
A CT scan is obtained with similar intervals as the ultrasound volume study. These two sets of images are then combined in such a way that the physics staff can determine the ‘post-plan’, or the actual radiation dose received by the prostate and surrounding region. This allows quality assurance and confirmation of a successful implant.
[to top]

